Will Posterior Tibial Tendon Dysfunction Involve Surgery Teatment ?
Overview
Adult acquired flatfoot deformity (AAFD), embraces a wide spectrum of deformities. AAFD is a complex pathology consisting both of posterior tibial tendon insufficiency and failure of the capsular and ligamentous structures of the foot. Each patient presents with characteristic deformities across the involved joints, requiring individualized treatment. Early stages may respond well to aggressive conservative management, yet more severe AAFD necessitates prompt surgical therapy to halt the progression of the disease to stages requiring more complex procedures. We present the most current diagnostic and therapeutic approaches to AAFD, based on the most pertinent literature and our own experience and investigations. 
Causes
Adult flatfoot typically occurs very gradually. If often develops in an obese person who already has somewhat flat feet. As the person ages, the tendons and ligaments that support the foot begin to lose their strength and elasticity.
Symptoms
Your feet tire easily or become painful with prolonged standing. It's difficult to move your heel or midfoot around, or to stand on your toes. Your foot aches, particularly in the heel or arch area, with swelling along the inner side. Pain in your feet reduces your ability to participate in sports. You've been diagnosed with rheumatoid arthritis; about half of all people with rheumatoid arthritis will develop a progressive flatfoot deformity.
Diagnosis
The diagnosis of tibialis posterior dysfunction is essentially clinical. However, plain radiographs of the foot and ankle are useful for assessing the degree of deformity and to confirm the presence or absence of degenerative changes in the subtalar and ankle articulations. The radiographs are also useful to exclude other causes of an acquired flatfoot deformity. The most useful radiographs are bilateral anteroposterior and lateral radiographs of the foot and a mortise (true anteroposterior) view of the ankle. All radiographs should be done with the patient standing. In most cases we see no role for magnetic resonance imaging or ultrasonography, as the diagnosis can be made clinically.
Non surgical Treatment
What are the treatment options? In early stages an orthotic that caters for a medially deviated subtalar joint ac-cess. Examples of these are the RX skive, Medafeet MOSI device. Customised de-vices with a Kirby skive or MOSI adaptation will provide greater control than a prefabricated device. If the condition develops further a UCBL orthotic or an AFO (ankle foot orthotic) could be necessary for greater control. Various different forms of surgery are available depending upon the root cause of the issue and severity. 
Surgical Treatment
Types of surgery your orthopaedist may discuss with you include arthrodesis, or welding (fusing) one or more of the bones in the foot/ankle together. Osteotomy, or cutting and reshaping a bone to correct alignment. Excision, or removing a bone or bone spur. Synovectomy, or cleaning the sheath covering a tendon. Tendon transfer, or using a piece of one tendon to lengthen or replace another. Having flat feet is a serious matter. If you are experiencing foot pain and think it may be related to flat feet, talk to your orthopaedist.
The Cause And Treatment For Posterior Tibial Tendon Dysfunction (PTTD)
Overview
Collapsed arches occur in five percent of adults 40 years and older, especially those who are overweight or maintain sedentary lifestyles. At the onset of the condition, adult acquired flatfoot can be controlled with anti-inflammatory medications, physical therapy, taping, bracing, and orthotics. While most cases of adult-onset flatfoot require surgery, congenital flatfoot is an entirely different condition that is best treated with orthotics in children. Ninety percent of children born with flat feet will be fine with conservative treatment. 
Causes
As discussed above, many health conditions can create a painful flatfoot. Damage to the posterior tibial tendon is the most common cause of AAFD. The posterior tibial tendon is one of the most important tendons of the leg. It starts at a muscle in the calf, travels down the inside of the lower leg and attaches to the bones on the inside of the foot. The main function of this tendon is to hold up the arch and support your foot when you walk. If the tendon becomes inflamed or torn, the arch will slowly collapse. Women and people over 40 are more likely to develop problems with the posterior tibial tendon. Other risk factors include obesity, diabetes, and hypertension. Having flat feet since childhood increases the risk of developing a tear in the posterior tibial tendon. In addition, people who are involved in high impact sports, such as basketball, tennis, or soccer, may have tears of the tendon from repetitive use. Inflammatory arthritis, such as rheumatoid arthritis, can cause a painful flatfoot. This type of arthritis attacks not only the cartilage in the joints, but also the ligaments that support the foot. Inflammatory arthritis not only causes pain, but also causes the foot to change shape and become flat. The arthritis can affect the back of the foot or the middle of foot, both of which can result in a fallen arch.
Symptoms
The symptoms of PTTD may include pain, swelling, a flattening of the arch, and an inward rolling of the ankle. As the condition progresses, the symptoms will change. For example, when PTTD initially develops, there is pain on the inside of the foot and ankle (along the course of the tendon). In addition, the area may be red, warm, and swollen. Later, as the arch begins to flatten, there may still be pain on the inside of the foot and ankle. But at this point, the foot and toes begin to turn outward and the ankle rolls inward. As PTTD becomes more advanced, the arch flattens even more and the pain often shifts to the outside of the foot, below the ankle. The tendon has deteriorated considerably and arthritis often develops in the foot. In more severe cases, arthritis may also develop in the ankle.
Diagnosis
It is of great importance to have a full evaluation, by a foot and ankle specialist with expertise in addressing complex flatfoot deformities. No two flat feet are alike; therefore, "Universal" treatment plans do not exist for the Adult Flatfoot. It is important to have a custom treatment plan that is tailored to your specific foot. That starts by first understanding all the intricacies of your foot, through an extensive evaluation. X-rays of the foot and ankle are standard, and MRI may be used to better assess the quality of the PT Tendon.
Non surgical Treatment
Conservative treatment is indicated for nearly all patients initially before surgical management is considered. The key factors in determining appropriate treatment are whether acute inflammation and whether the foot deformity is flexible or fixed. However, the ultimate treatment is often determined by the patients, most of whom are women aged 40 or older. Compliance can be a problem, especially in stages I and II. It helps to emphasise to the patients that tibialis posterior dysfunction is a progressive and chronic condition and that several fittings and a trial of several different orthoses or treatments are often needed before a tolerable treatment is found. 
Surgical Treatment
If initial conservative therapy of posterior tibial tendon insufficiency fails, surgical treatment is considered. Operative treatment of stage 1 disease involves release of the tendon sheath, tenosynovectomy, debridement of the tendon with excision of flap tears, and repair of longitudinal tears. A short-leg walking cast is worn for 3 weeks postoperatively. Teasdall and Johnson reported complete relief of pain in 74% of 14 patients undergoing this treatment regimen for stage 1 disease. Surgical debridement of tenosynovitis in early stages is believed to possibly prevent progression of disease to later stages of dysfunction.
Posterior Tibial Tendon Dysfunction (PTTD)
Overview Adult acquired flatfoot deformity (AAFD) is a painful, chronic condition found most often in women between the ages of 40 and 60. AAFD occurs when the soft tissues of the foot are overstretched and torn, causing the arch to collapse. Flatfoot deformities may also be caused by a foot fracture, or may result from long-term arthritis. Once the posterior tibial tendon-the tendon unit that holds up the arch-loses its function, the foot becomes ?flat? as the bones spread out of position during weight bearing. Without an AAFD repair, the condition may progress until the affected foot becomes entirely rigid and quite painful. 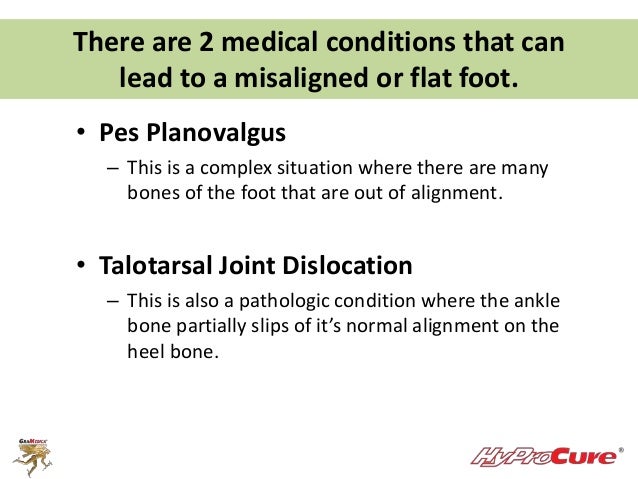 Causes Rheumatoid arthritis This type of arthritis attacks the cartilage in the foot, leading to pain and flat feet. It is caused by auto-immune disease, where the body?s immune system attacks its own tissues. Diabetes. Having diabetes can cause nerve damage and affect the feeling in your feet and cause arch collapse. Bones can also fracture but some patients may not feel any pain due to the nerve damage. Obesity and/or hypertension (high blood pressure) This increases your risk of tendon damage and resulting flat foot. Symptoms Not everyone with adult flatfoot has problems with pain. Those who do usually experience it around the ankle or in the heel. The pain is usually worse with activity, like walking or standing for extended periods. Sometimes, if the condition develops from arthritis in the foot, bony spurs along the top and side of the foot develop and make wearing shoes more painful. Diabetic patients need to watch for swelling or large lumps in the feet, as they may not notice any pain. They are also at higher risk for developing significant deformities from their flatfoot. Diagnosis The diagnosis of tibialis posterior dysfunction is essentially clinical. However, plain radiographs of the foot and ankle are useful for assessing the degree of deformity and to confirm the presence or absence of degenerative changes in the subtalar and ankle articulations. The radiographs are also useful to exclude other causes of an acquired flatfoot deformity. The most useful radiographs are bilateral anteroposterior and lateral radiographs of the foot and a mortise (true anteroposterior) view of the ankle. All radiographs should be done with the patient standing. In most cases we see no role for magnetic resonance imaging or ultrasonography, as the diagnosis can be made clinically. Non surgical Treatment Orthotic or anklebrace, Over-the-counter or custom shoe inserts to position the foot and relieve pain are the most common non-surgical treatment option. Custom orthotics are often suggested if the shape change of the foot is more severe. An ankle brace (either over-the-counter or custom made) is another option that will help to ease tendon tension and pain. Boot immobilization. A walking boot supports the tendon and allows it to heal. Activity modifications. Depending on what we find, we may recommend limiting high-impact activities, such as running, jumping or court sports, or switching out high-impact activities for low-impact options for a period of time. Ice and anti-inflammatory medications. These may be given as needed to decrease your symptoms.
Causes Rheumatoid arthritis This type of arthritis attacks the cartilage in the foot, leading to pain and flat feet. It is caused by auto-immune disease, where the body?s immune system attacks its own tissues. Diabetes. Having diabetes can cause nerve damage and affect the feeling in your feet and cause arch collapse. Bones can also fracture but some patients may not feel any pain due to the nerve damage. Obesity and/or hypertension (high blood pressure) This increases your risk of tendon damage and resulting flat foot. Symptoms Not everyone with adult flatfoot has problems with pain. Those who do usually experience it around the ankle or in the heel. The pain is usually worse with activity, like walking or standing for extended periods. Sometimes, if the condition develops from arthritis in the foot, bony spurs along the top and side of the foot develop and make wearing shoes more painful. Diabetic patients need to watch for swelling or large lumps in the feet, as they may not notice any pain. They are also at higher risk for developing significant deformities from their flatfoot. Diagnosis The diagnosis of tibialis posterior dysfunction is essentially clinical. However, plain radiographs of the foot and ankle are useful for assessing the degree of deformity and to confirm the presence or absence of degenerative changes in the subtalar and ankle articulations. The radiographs are also useful to exclude other causes of an acquired flatfoot deformity. The most useful radiographs are bilateral anteroposterior and lateral radiographs of the foot and a mortise (true anteroposterior) view of the ankle. All radiographs should be done with the patient standing. In most cases we see no role for magnetic resonance imaging or ultrasonography, as the diagnosis can be made clinically. Non surgical Treatment Orthotic or anklebrace, Over-the-counter or custom shoe inserts to position the foot and relieve pain are the most common non-surgical treatment option. Custom orthotics are often suggested if the shape change of the foot is more severe. An ankle brace (either over-the-counter or custom made) is another option that will help to ease tendon tension and pain. Boot immobilization. A walking boot supports the tendon and allows it to heal. Activity modifications. Depending on what we find, we may recommend limiting high-impact activities, such as running, jumping or court sports, or switching out high-impact activities for low-impact options for a period of time. Ice and anti-inflammatory medications. These may be given as needed to decrease your symptoms.  Surgical Treatment Types of surgery your orthopaedist may discuss with you include arthrodesis, or welding (fusing) one or more of the bones in the foot/ankle together. Osteotomy, or cutting and reshaping a bone to correct alignment. Excision, or removing a bone or bone spur. Synovectomy, or cleaning the sheath covering a tendon. Tendon transfer, or using a piece of one tendon to lengthen or replace another. Having flat feet is a serious matter. If you are experiencing foot pain and think it may be related to flat feet, talk to your orthopaedist.
Surgical Treatment Types of surgery your orthopaedist may discuss with you include arthrodesis, or welding (fusing) one or more of the bones in the foot/ankle together. Osteotomy, or cutting and reshaping a bone to correct alignment. Excision, or removing a bone or bone spur. Synovectomy, or cleaning the sheath covering a tendon. Tendon transfer, or using a piece of one tendon to lengthen or replace another. Having flat feet is a serious matter. If you are experiencing foot pain and think it may be related to flat feet, talk to your orthopaedist.